Patients will often withhold information from their medical providers for numerous reasons. It could either be due to the embarrassment, the idea that it may not be important, the fear of getting into trouble, or protecting someone else. There were reasons all across the board. It can be quite difficult for medical providers to properly treat a patient if patients do not inform providers of all the circumstances. Medical providers are not there to judge the patient. They are not there to scold patients for their actions. They are here to make sure that their patients are alive and okay. Tattling does not come with our job titles.

But as a 13 year old in middle school, I can see why medical professionals seem scary -especially in front of parents.
It was another afternoon in the ER when we met our 13 year old male patient who was accompanied by his mother for abdominal pain. More specifically, the pain was regional to the left-sided flank area with no associated symptoms. The initial suspicion for flank pain is usually kidney stones. Although kidney stones are more common in adults (for numerous reasons such as certain prescription medications or dehydration), it is not rare for teenagers. The patient, a fairly skinny boy, looked distressed. He was squirming in his chair and relied on his mother to speak with the doctors. I can’t judge him though. I used to be a shy kid too.

Our patient was having a regular day at school when he started feeling pain near his right hip. The pain was consistent, non-radiating, and was not relieved by any factors. The mother was concerned because the patient woke up completely fine and went to school without any complaints. She gave her son Pepto Bismal when he came home from school as they suspected he had an upset stomach from the school lunch. The thought of having to consume school lunch made even my stomach turn. Unfortunately, the pain persisted, which prompted the mother to bring her son to the ER for further evaluation.

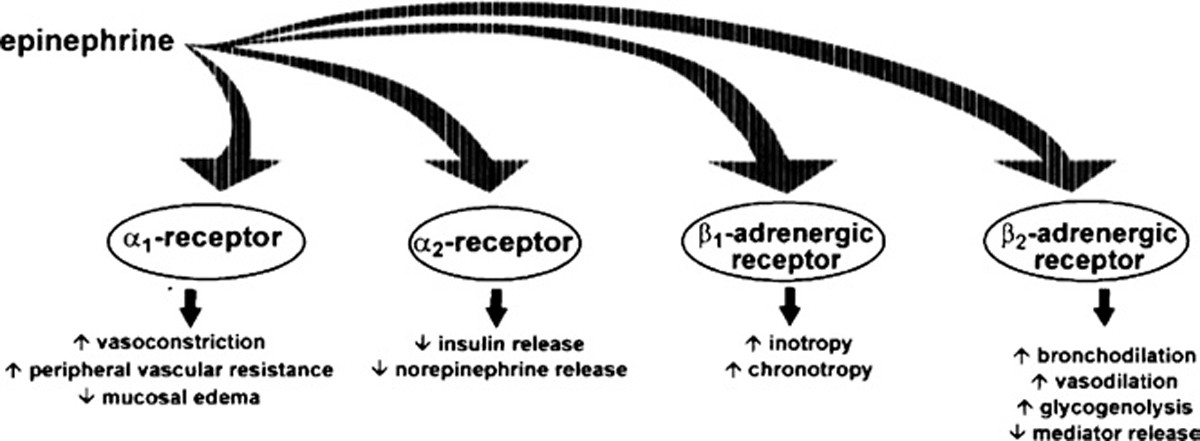
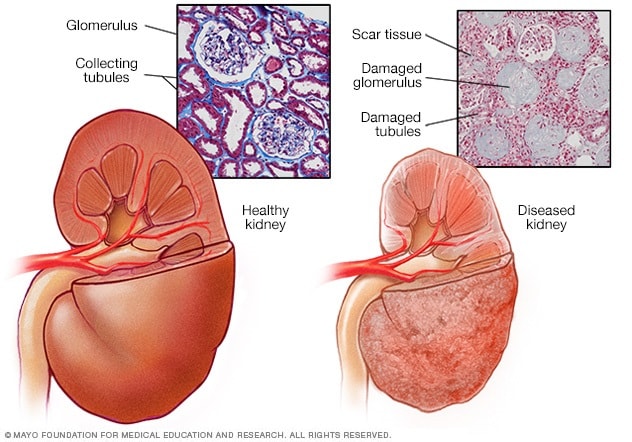
Indicators of kidney stones are typically severe abdominal pain, nausea, vomiting, and dysuria (pain with urination). Many individuals may also experience hematuria (blood in the urine). Abdominal pain can be caused for numerous reasons. The best way to determine the etiology of the abdominal pain, or any medical concern for that matter, is first through the history obtained from the patient. In this case, there were no outside factors that were contributing to this patient’s abdominal pain. The patient did not consume any takeout or new food this past week to suggest an upset stomach. The lack of fever, nausea, and vomiting ruled out a possible bacterial infection. There were also no recent injuries that could account for the abdominal pain. Considering all viewpoints, the next test would be a urinalysis. A urine sample can result in multiple findings: for kidney-related issues, physicians will look for red blood cells that indicated hematuria, crystals, and trace minerals that could lead to stone formation, white blood cell elevation to account for infections (especially urinary tract infections) and also increases in the urine pH which can also indicate kidney stones. It is not necessary for all of those elements to come back positive to suggest kidney stone formation, but it will give the physician enough evidence to start treating the condition properly and effectively. To our surprise, the urinalysis was completely normal.

So what was going on?
Pain medication that was supposed to alleviate the abdominal pain was not working. In fact, the patient was complaining of increasing abdominal pain which was now associated with dysuria. Things were just not adding up. No infection. No stones. No food poisoning. And certainly no indication for discharge. This meant further testing.
The mother at this point was frustrated with the 2-hour duration of the ER visit. She wanted to go home and see if her son could just sleep it off. The patient looked tired too. But the risk of missing something significant was not worth it. The physician decided to obtain a CT scan of the abdomen for further investigation. Perhaps there were small salt deposits that were in the kidneys that were not picked up by the labs, but could potentially be seen through a scan.
We got the scans back and it was a finding that the physician would not have considered given the initial history. He asked the mother if it was okay to step outside of the room so that he could speak to the patient in private.
Doctor: “Hey, how are you feeling?”
Patient: “Not so good. Nothing changed”.
Doctor: “I’m sorry to hear that. Is there anything you would like to share with me that you didn’t feel comfortable sharing in front of your mom?
The patient hesitated for a minute. He started to shake his head when the physician interrupted.
Doctor: “You’re not gonna get in trouble, that’s my promise to you. But I can’t help you feel better if I don’t know the full story”
Patient: “We were in gym class and I was joking around with my friends and this girl accidentally punched me.”
Doctor: “That must have been one strong accidental punch. Can I invite your mother back in?”
The boy looked down and nodded.
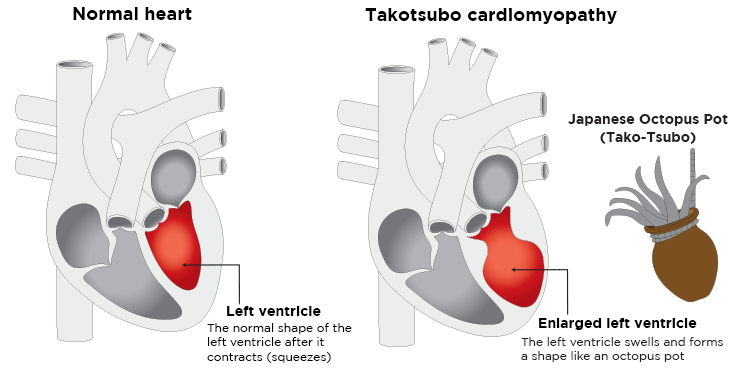
“Your son’s left kidney appears dented on the scan. This is usually the result of a blunt force trauma.”

The mother looked confused- rightfully so. The patient was not in a car accident, nor was he injured by any blunt force object.
“He actually got punched, accidentally, on the left side of his abdomen. Due to his small frame and low weight he was punched hard enough to sustain an injury to the kidney. We’re going to transfer him to the pediatric ER for further management.”
The mother looked horrified and confused. Although the patient wasn’t at any immediate risk, it was important to monitor his kidneys to prevent any future renal complications which could include dysuria, hematuria, infection, etc. Most cases, like this, will be treated non-operatively. Non-invasive treatments such as checking vitals, urine cultures, and lab work that assesses the function of the kidneys are necessary to clear the patient for discharge. Bed rest is also crucial in making sure the body can recover from the added stress.
While it was a long ER visit and an even longer story, it seemed like our patient’s friend got the punchline wrong.

Sources:
https://jamanetwork.com/journals/jamapediatrics/fullarticle/2442837
https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-stones/diagnosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6120183/












![cute cartoon kidney and doctor - Stock Illustration [27114247] - PIXTA](https://en.pimg.jp/027/114/247/1/27114247.jpg)