Epinephrine is more than just a hormone; it may save your life one day.
Also known as “adrenaline”, epinephrine is produced by the adrenal medulla to activate the sympathetic nervous system in response to physical and emotional stressors. But did you know that epinephrine is also one of the top ten most commonly used medications in critically ill patients?

Epinephrine can be used to treat a multitude of systemic dysfunctions but is most commonly used to treat anaphylaxis and cardiac arrest (including pulseless ventricular tachycardia, pulseless electrical activity, ventricular fibrillation).
Anaphylaxis is the rapid onset of a life-threatening severe allergic reaction that requires proper medical attention. This allergic reaction can be triggered by food, insect bite, chemical exposure, or even medication. The symptoms can range from diffuse erythema(redness), itchiness and hives, angioedema (swelling underneath the skin), to as serious as laryngeal edema (swelling of the larynx), difficulty breathing caused by bronchospasm, hypotension (low blood pressure), cardiac irregularities, syncope (loss of consciousness), and shock. Since anaphylaxis can quickly worsen and target multiple organ systems, epinephrine is given first due to its rapid response in comparison to the antihistamines and corticosteroids. Medical providers will inject epinephrine intramuscularly (EPI IM) into the anterolateral aspect of the thigh due to its quick absorption.

So, what exactly does epinephrine do in this case? Well, epinephrine has both alpha- and beta-adrenergic receptors which both work together to bring down the symptoms of anaphylaxis. In larger doses, the alpha-adrenergic receptors are favorable. The alpha-adrenergic receptor reverses the vasodilation by endorsing vasoconstriction which increases the blood pressure and improves the body’s state of hypotension. It also minimizes the diffuse erythema, angioedema, and hives. Working with the alpha-adrenergic receptor, the beta-adrenergic receptor addresses the bronchospasms by dilating the bronchial airways which improve any difficulty with breathing, increases the myocardial muscle contraction (heart contracts more), and increases heart rate. Figure one shows the break down of the multi-adrengergic properties.
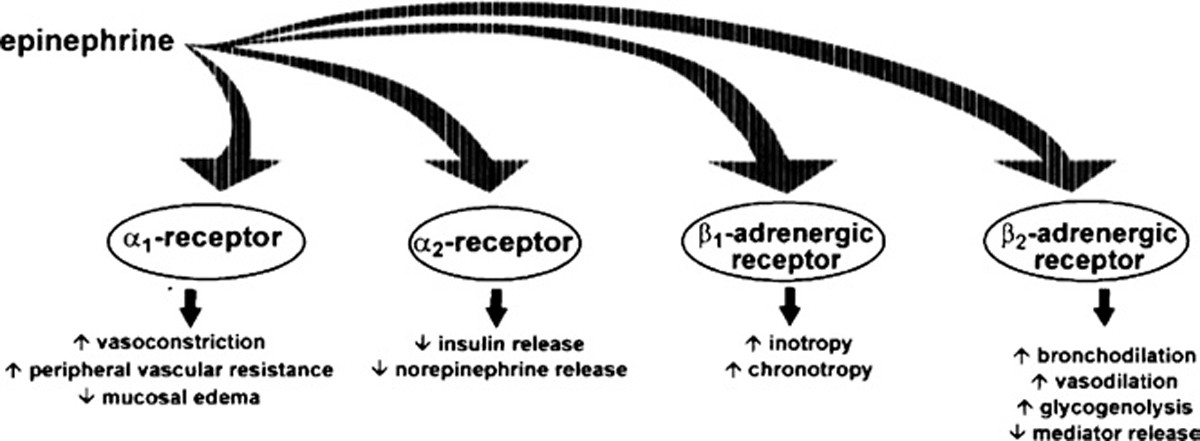
Image source https://link.springer.com/article/10.1186/1939-4551-1-S2-S18
By managing these symptoms, the providers avoid the risk of the patient going into cardiac arrest. After the epinephrine is administered, providers will then start on antihistamines and corticosteroids as the epinephrine stabilizes the symptoms. While epinephrine has a rapid onset, it does have a short duration of action which is why patients can be given several doses of epinephrine every 5-15 minutes until symptoms improve.
Let’s say that instead of initially injecting epinephrine the patient was started on an antihistamine such as Benadryl. By the time that Benadryl can start acting on the symptoms, the symptoms can worsen and begin targeting other organ systems with worsening conditions. In that case, the patient may go into anaphylactic shock or cardiac arrest which then becomes a life-threatening medical emergency.
As I mentioned above, epinephrine is typically injected IM. During urgent situations in which a patient is either unconscious due to a severely hypotensive state, does not respond to IV fluids, or goes into cardiac arrest, the medical providers will administer a higher dose of epinephrine intravenously (IV EPI) which reacts immediately.

The reason medical providers only administer epinephrine intravenously is due to the risk factors it may cause. As the patient is in a “life or death” situation, the benefits of IV EPI outweigh the risks. These patients are also heavily monitored and likely have an IV set up upon their initial admission into the hospital. In general, common side effects of epinephrine include nausea, vomiting, agitation, tremors, dizziness, palpitations, and headaches. Some possible side effects of IV EPI can include myocardial infarction (heart attack), pulmonary edema (fluid in lungs), intracranial hemorrhage (brain bleed), and cardiac irregularities. But that being said, not every patient who receives IV epinephrine will endorse any of these risk factors. Since these critically-ill patients are continuously monitored, they will also be treated for any adverse reactions of any treatments that are given. They have to save your life first, right?
If you have any food allergies, you may carry around an Epi-Pen. If you didn’t already know, an Epi-Pen is a fixed dose of either 0.15mg or 0.30mg of epinephrine that you inject into your body during an allergic reaction. Rather than carrying around a syringe and vial of epinephrine, you can carry around a pen that can be safely injected into your body if you accidentally consume peanut butter.

Whether it is a terrible allergic reaction or an intense battle against death, it is fascinating to see how a hormone can be the answer. It really shows that every single aspect of your body is far more complex than you can imagine and they all work together to make sure you’re functioning and staying alive.
So yes, epinephrine for the win.
References:
FER. Simons, ZH. Chad, et al. “Epinephrine: The Drug of Choice for Anaphylaxis–A Statement of the World Allergy Organization.” World Allergy Organization Journal, BioMed Central, 1 Jan. 1973, link.springer.com/article/10.1186/1939-4551-1-S2-S18.
Wood, Joseph P, et al. “Safety of Epinephrine for Anaphylaxis in the Emergency Setting.” World Journal of Emergency Medicine, Second Affiliated Hospital of Zhejiang University School of Medicine, 2013, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4129903/#:~:text=Because%20of%20the%20potential%20for,multiple%20IM%20doses%20of%20epinephrine.
