Many of us can say that we have dealt with pesky ingrown hairs and even went ahead to try and resolve it on our own. While some people were wise enough to seek a medical professional to do this job, others (yes, including myself) have done it on our own with a pair of tweezers. Some resort to just squeezing it out with their fingers. Whatever the method, if it is not done with sterile materials, the aftermath can be nastier than the ingrown itself.
The ingrown hair usually resolves on its own, unless it is too painful and needs extraction. If you attempt to remove an ingrown hair without being careful, it can lead to an ER visit.
This brings me to a very entertaining, but equally jaw-dropping patient scenario in which a 24-year-old female patient presented to the ER with 1 week of worsening left leg swelling, pain, redness, intermittent numbness and 2 days of low-grade fevers. Just by looking at the patient’s leg, you could tell that this patient was not off to a good start.
The Story:
“So…I had a pimple on my leg and I ran my razor over it to shave it off. It was the kind of pimple that has a hair stuck under it – even though I tried shaving over it several times. It looked a little red after shaving, so I applied some perfume.”
We had to ask, why the perfume?
“Perfume has some alcohol in it and that is supposed to be good for wounds, right?”
Yes…but no. Alcohol does sterilize a wound however, perfume is a mix of several different chemicals and fragrances that can irritate the skin. When perfume is applied to a fresh wound, despite the size of the wound, the skin can become inflamed and irritated. There can also be watery or purulent discharge (white or yellow) from the area.
The patient continues her story stating “the little bump was still red so I put some Neosporin on it, but then noticed it expired a few months ago.”
Yikes…expired Neosporin? At first, the expired product did seem like a red flag however, research shows that Neosporin can still be effective one year past its shelf-life. Expired Neosporin just isn’t as effective.
As the patient’s small little ingrown hair worsened, the redness and warmth began to slowly spread up her left leg.
Now we all know that mothers just happen to know home remedies for just about any medical concern and when things go wrong, mothers know best. The patient’s mother made her an herbal salve to apply to the wound area which was soothing for a short amount of time, but nowhere near resolving the issue.
The patient began to get worried. Her entire left leg was swollen with streaking redness traveling up the leg. She also experienced periods of leg numbness. Her left leg was warm to touch and painful too. She told us she did not take any pain medication and was hoping the symptoms would resolve with time. The patient started having low-grade fevers about a week after the initial symptoms.
“I was concerned because things were getting worse instead of better. I went on google which said I need to amputate my leg and I also called my friend because I’m scared. Do I really need to amputate my leg? My friend told me to come to the ER immediately. I waited one more day just to be sure and because I don’t have insurance. What if I was just overreacting.”

The Diagnoses:
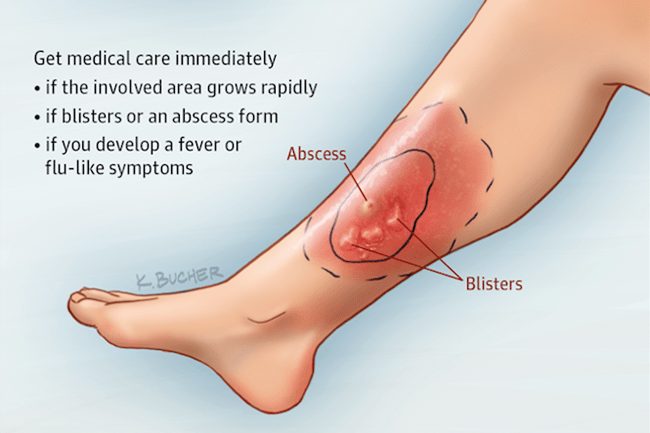
The patient’s small little wound was a case of cellulitis, a rather common bacterial infection of the skin and soft tissue. Cellulitis is treatable with oral antibiotics and can be resolved in about a week if symptoms are mild.
Cellulitis is caused by the staph and strep bacteria which infects the skin and tissue. When cellulitis goes untreated, the infection can spread and cause tissue death. The infection can spread to the bone, trigger sepsis (blood infection), and can affect the lymphatic and nervous system. In these dangerous cases, the patient will need to be admitted to the hospital for further treatment and care management. An amputation may be required if cellulitis is in the bones and needs to be stopped before it travels to the blood or major organs. Sometimes, patients will also need surgery to remove any dead tissue or to remove the infected tissue to prevent the spread. Cellulitis is a higher risk for elderly or diabetic patients. At times the presentation of cellulitis can be misinterpreted for diabetic foot, dermatitis, DVT, or other similar etiologies. It is better to be safe and have your symptoms checked out.
Cellulitis can be triggered by an open wound, animal bite, infected surgical site, skin breaks due to eczema or athlete’s foot, IV drug use. If you do have an open wound or skin break that is at risk for infection, it is best to keep that area clean and dry. The CDC recommends avoiding hot tubs, beaches/rivers/lakes, and swimming pools if you do have an open wound.

The Lesson:
Thankfully, the 24-year-old patient was able to fully recover with IV antibiotics with no need for surgery or amputation. If she had waited longer, who knows what her prognosis would have been!
It was indeed an ingrown gone wrong.
References:
“Cellulitis.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 29 May 2020, http://www.cdc.gov/groupastrep/diseases-public/Cellulitis.html.
Cranendonk DR, Lavrijsen APM, Prins JM, Wiersinga WJ. Cellulitis: current insights into pathophysiology and clinical management. Neth J Med. 2017;75(9):366-378.