After some observation, I’ve come to the conclusion that the kidneys are in fact the most dramatic organs. Your body could be dealing with an issue such as a pulmonary embolism and your kidneys will somehow manage to steal the spotlight. These are all just observations though…I’ll have to do some further investigating before I can add more dirt for those kidneys to filter out. It just goes to show how the human body functions as a whole system, rather than separate systems.
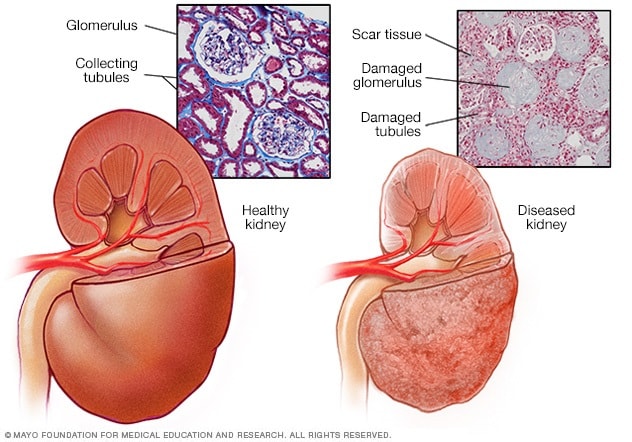
Kidneys have a lot on their plate. The kidneys balance the body by filtering out excess fluid, removing waste, regulating blood pressure, and monitoring red blood cell production. Unfortunately, 8-16% of the world population suffer from Chronic Kidney Disease (CKD) or End-Stage Renal Disease (ESRD) . It is also the most prevalent disorder among the geriatric community. CKD is the progressively worsening kidney function which requires renal therapy, kidney transplant, or dialysis. While the wait for a kidney transplant can be long or even risky for many patients with comorbidities, dialysis is the more desirable treatment plan.
The Artificial Kidney
Dialysis is the renal treatment that acts as an “artificial kidney” and filters out the toxins of the body. While it can help facilitate one of the functions of the kidneys, dialysis cannot “replace” the kidneys or fulfill complete performance. There are two types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis is completed through a dialyzer, a machine that acts as an artificial kidney apparatus outside of the body in order to filter out the toxins and excess wastes. This treatment is most often done at a dialysis center at least 3 times per week, depending on the patient’s conditions. Home hemodialysis can also be done if the patient has the equipment and medical staff. Peritoneal dialysis is more favorable for younger patients as it uses the peritoneal membrane as a filter which allows treatments to be done directly at home.

Dialysis Prep
Prior to starting the hemodialysis treatment, a patient will need to have an AV- fistula or shunt in the forearm. The AV fistula is a surgical procedure that creates a larger blood vessel by combining a vein and artery together in the forearm. It is important to create this AV shunt as it allows muscle to grow around the vein and making it as strong as an artery to withstand several punctures throughout the dialysis treatments. This blood vessel is necessary in order to insert the dialysis cannulas.
The Process of Hemodialysis
So you may be asking, what exactly happens when a patient is undergoing dialysis? The dialysis cannulas is inserted into the patient’s AV fistula at the time of hemodialysis. This links the patient’s blood with the dialyzer, the external filter that has a semipermeable membrane. As the blood flows out of the body and into the dialyzer, there is a counter-current flow gradient in which the blood goes through the semipermeable filter while the dialysis fluid goes in the opposite direction. Through diffusion, the metabolic wastes such as urea and creatinine diffuse into the dialyzer fluid, while the filtered blood remains in the filter to go back into the body. The dialysis fluid is a chemical mixture of acid concentrate, deionized water, NaHCO3 and NaCl that is created specifically for the patient to ensure the best results. This is monitored by rechecking labs and vitals during and after the dialysis treatment. If there needs to be any changes to the fluid, the nephrologist can adjust the balance of the chemicals. The rate of diffusion depends on the size of waste particles. The larger the molecules, the longer the diffusion process will take. Typically, patients will have 4 hour treatments at the dialysis center during the day. Some patients prefer to have their dialysis treatments at night, which gives him more free-time during the day. Since the nighttime dialysis is a longer period of time, the days are free for patients to carry on their daytime activities, go to work, and have a less restrictive diet. Our kidneys work non-stop all hours of the day to make sure our blood is constantly filtered. Dialysis patients only get 4 hours of that filtration, rather than the full 24 hours. Longer dialysis treatments allow patients to get more of that kidney function they are missing.

The Process of Peritoneal Dialysis
Unlike hemodialysis, peritoneal dialysis is an internal filtration process that takes place in the abdominal cavity. Most peritoneal patients can do the process at home and have monthly follow ups with their nephrologist to ensure the process is going smoothly. Much like hemodialysis, patients who choose to have peritoneal dialysis will need surgery for a permanent abdominal catheter. The catheter is necessary to insert 2 liters of dialysis fluid that is routinely replaced with new fluid. The fluid can either be replaced every 3-4 hours manually which is known as the continuous ambulatory peritoneal dialysis (CAPD). There is always fluid in the abdominal cavity with peritoneal dialysis. Patients who choose this process require training on how to maintain catheter hygiene in order to prevent infections. If the patient is unable to change out the fluid due to a busy day schedule, they can choose the automated peritoneal dialysis (APD) option to do at night. APD is when the patient connects the abdominal catheter to a small machine called a cycler that replaces the fluid while the patient is asleep. Both options offer more freedom and are time-friendly compared to hemodialysis as they do not require going to a dialysis center 4 hours every 3-5 days.

The Risks of Dialysis
With any treatment, there are risks which we cannot avoid. Ultimately, we weight the benefits and the risks to see if the treatment is worth it. Leading up to the decision to start dialysis, the body is also inflamed due to oxidative stress from accumulation of waste and toxins in the blood. As the kidney function declines, the kidneys begin to release macrophages, glomerular cells, and vascular cells to produce free radicals which add to the oxidative stress. The oxidative stress not only affects the kidneys, but also major organs which can lead to hypertension, anemia, hyperlipidemia, cardiovascular disease, lack of appetite, and muscle aches. When dialysis treatments begin, there is a risk of blood clotting, AV shunt site infection, hypotension, and issues with the thyroid. The AV shunts is prone to infection as it is the primary source of insertion. It is important to check the shunt to make sure there isn’t any heavy bleeding after a treatment or any signs of infection. Patients with peritoneal dialysis are more susceptible to peritonitis, the infection of the peritoneal lining from bacteria in the catheter. There is also a chance the tubes within the abdomen can stick together or get stuck which can either make dialysis more difficult or stop it immediately. Despite these risks, patients are often set on receiving dialysis as it improves quality of life. These side effects are all treatable and can be prevented with the right precautions.

Patients can interchange between methods of dialysis. They can start off with hemodialysis then switch over to peritoneal dialysis and vice versa. These options are thoroughly discussed between the patient and doctors for the best option and the patient’s well being. Some people even choose to stop dialysis all together. When this is the case, the patient’s medical team will help with the transition and help the patient medically, because at the end of the day, healthcare is about supporting the patient’s health and respecting their choices.
![cute cartoon kidney and doctor - Stock Illustration [27114247] - PIXTA](https://en.pimg.jp/027/114/247/1/27114247.jpg)
An Open Letter To Our Kidneys
Dear kidneys, please don’t act up. We have treatments to mimic some of your functions, but at the end of the day you are still the stars below our ribs.
References
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Dialysis in chronic kidney disease. 2018 Mar 8. Available from: https://www.ncbi.nlm.nih.gov/books/NBK492979/
“Hemodialysis.” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, 1 Jan. 2018, http://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis.
Vadakedath, Sabitha, and Venkataramana Kandi. “Dialysis: A Review of the Mechanisms Underlying Complications in the Management of Chronic Renal Failure.” Cureus, Cureus, 23 Aug. 2017, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5654453/.